Healthcare systems are at the frontline of delivering critical care during emergencies. From flood-induced cholera outbreaks to earthquake casualties and zoonotic diseases, health care systems play a crucial role in mitigating the illnesses and deaths caused by emergencies.
Countries’ ability to provide reliable essential healthcare during emergencies is critical to protect people’s lives. For example, World Health Organization data for 80 countries show that around 1.4 million fewer people received necessary care for tuberculosis in 2020 from a year ago from pandemic disruptions.
Large systemic shocks — like pandemics or natural disasters — highlight the urgent need for resilient health systems for mitigating the loss of lives and prolonged impacts on people’s livelihoods. To effectively serve patients during normal times, health care providers need adequate facilities, equipment, staff, medical supplies, food supply, information management capabilities, and reliable access to power and clean water. In addition, well-established governance and institutional mechanisms and policies are fundamental to enable emergency responses during pandemics or natural disasters.
GFDRR’s Frontline report draws attention to the importance of the interdependence of health systems and other sectors, particularly infrastructure systems and broader emergency response and fiscal governance frameworks. The Frontline report documents case studies that highlight the foundational role that quality infrastructure systems in addition to human resources and management play for a functioning health care system — including reliable water, electricity, and transport. The effective response to pandemics and/or natural disasters depends not only on the health care system itself, but also on its supporting lifeline infrastructure.
The Climate & Disaster Resilient Health Systems thematic area contributes to strengthening the resilience of health systems and their enabling environment to a wide range of emergencies. It will generate targeted knowledge, tools and operational analytics that identify critical gaps and opportunities in countries’ health systems and prioritize measures that can be leveraged for resilient investments in countries.
Highlights

Watch the Climate and Disaster Risk Management for Health Systems videos playlist on YouTube
The Climate & Disaster Resilient Health Systems thematic area provides analytical and advisory services to support client countries.
Even before the COVID-19 pandemic, healthcare systems in many World Bank client countries were struggling to meet routine demand; let alone being able to effectively manage emergencies. But the needs that have emerged during the pandemic are highlighting and intensifying these existing challenges – especially when it comes to capacity, coordination, and effective system planning.
Large shocks – like pandemics or natural disasters – have also shown that simply buying more hospital beds or equipment is not enough to make health systems resilient. Through this thematic area, the World Bank is drawing on its expertise in disaster risk management and public health to offer integrated solutions – integrating health and emergency response agencies, and strengthening the infrastructure on which healthcare systems depend.
GFDRR’s Frontline report makes concrete recommendations for how to increase the resilience of health systems to emergencies. It translates established disaster risk management principles of preparedness, risk reduction, response into actions for the health sector. It also introduces a resilient infrastructure (Lifelines) perspective to health: hospitals can’t function without reliable energy/water; patients can’t access healthcare without resilient transport.
The area’s activities center around five priority areas that were highlighted in the Frontline report:
- Strengthen foundations of resilient health service delivery: A wide range of enabling factors need to be strengthened, such as adequate equipment, financing, skilled staff, effective information systems, and efficient management and operational protocols. Continued investments and policy actions are essential to ensure that health systems can offer inclusive, affordable, and quality services.
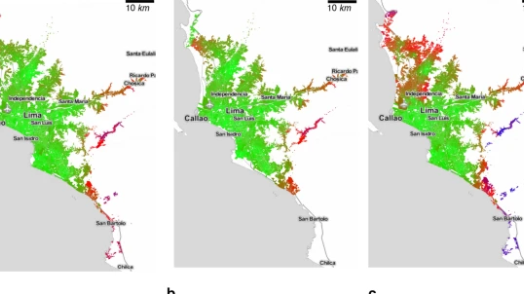
- Increase resilience of health facilities: Contingency planning can be key to prepare the capacity, skills, staff, equipment, management, supplies, and protocols needed for emergency contexts. Healthcare facilities themselves must also be resilient to shocks, such as floods or earthquakes.
- Strengthen the resilience of overall health systems: When resources are limited, it is impossible to immediately equip every facility to the highest standard. Enhanced communication channels and use of digital health, data-driven approaches for coordinated service delivery, and mobile clinics can help to meet surge demand through a system-level and regionally coordinated response. This also includes anticipating resource and capacity constraints and having contingency plans for critical supply needs.
- Improve coordination: The emergency preparedness of health systems needs to be closely coordinated with a country’s overall emergency management and disaster response systems, such as the military, civil protection, and community groups, with clearly defined roles and mandates for crisis response. This is paramount when basic needs (food, shelter, etc.) and public services (security, social safety nets, healthcare, etc.) must be provided simultaneously in post-disaster situations.
- Invest in resilient infrastructure: Quality infrastructure is essential for effective healthcare services—even more so during disasters and pandemics. Resilient water, electricity, transport, and communication and digital systems are crucial to ensure adequate treatment capacity, equitable access to healthcare, and the functioning of supply chains. The resilience of healthcare services depends on the interdependence of these lifelines.